Depression - the most common mental disorders, the growth rate of their prevalence in recent decades, rapid. The incidence of depression is approaching 3%, and the risk of getting sick throughout life is 20%. The prevalence of depressive disorders among men is 4-10%.
The relationship of depression with pathology in the sexual sphere has been the subject of attention of many generations of domestic and foreign researchers. R. Krafft-Ebing wrote that a patient in a depressive state ceases to have desires, since any goal seems to him unattainable and that "the consciousness and mood of melancholic are unfavorable for the awakening of sexual desire." S. Freud noted: "A particularly powerful asthenizing factor in affective disorders with sexual disorders is switching the entire mental register of the individual to the area of extreme anxiety about reducing or losing one's masculinity." Speaking about the relationship of depression and sexual dysfunction, it should be noted that at the dawn of sexological studies, greater importance was attached to sexual dysfunction itself, and mood disorders were considered their consequence. And only by the end of the XIX century, violations in the sexual sphere began to be considered not as a cause, but as a consequence of mental illness. This began to concern primarily the works on the psychosomatic aspects of depressive disorders, masked depressions and somatic equivalents of depressions, in which sexual dysfunctions were described as manifestations of impaired autonomic nervous system function.
Prevalence of sexual dysfunctions in depressive disorders
Data on the prevalence of sexual disorders in a population vary greatly from 2 to 50% in various forms depending on gender and age. In this regard, it should be noted that epidemiological studies in the field of sexopathology meet certain difficulties. The fact is that information, both obtained by direct examination of patients, and coming from various medical institutions, is not reliable enough. This is due to the fact that, firstly, patients often hide their sexual dysfunction, secondly, the data obtained depend on the clinical qualifications and orientation of the researcher, thirdly, there are serious differences in diagnostic issues among sexopathologists belonging to different schools and there are also significant differences in research methods.
In general, the frequency of sexual problems in patients with depression is about 2-3 times higher than in the general population - 50% compared with 24%. According to some authors, 5% of men with depression experience difficulties due to reduced sexual desire, 21-38% suffer from premature ejaculation and 4-10% suffer from orgasmic disorders. The data presented in the study N.Sh. Tatlaeva, indicate a significant prevalence of disorders of libido, erection, ejaculation, orgasm, and the level of sexual activity in general in depressed patients. According to the literature, the libido to one degree or another decreases in 100% of cases, the level of sexual activity - in 99%, erection - in 98%, and orgasm - in 82%. However, as mentioned above, there is a fairly large range of indicators, which is explained by the unspecified treatment of patients for sexological assistance that does not reflect the true prevalence of disorders in the population. Only very degraded patients with a "complete lack of modesty" can bring the details of their intimate life to the doctor's attention. For the majority, communication with a doctor on this topic presents great difficulties. This is evidenced by the fact that among the 6,000 Western Germans who tried to commit suicide, more than had some sexual problems, and in 21% they were the main motive, and in 32% they were one of the most important. J. Hempel et al. reported that impotence ranks second among the motives for suicide. To this we can add that the patient's sexual problems are a very unpleasant topic for doctors, especially women.
The modern view of the relationship of sexual and depressive disorders
It is known that depression is characterized by a number of somatic disorders, biochemical changes, and hormonal changes. Do not make exceptions and violations in the sexual sphere. According to some foreign authors, depression has a marked decrease in sexual desire, erectile dysfunction and ejaculation occur, and the ability to enjoy sexual fantasies is lost. V.D. Topolyansky emphasizes that functional sexual disorders are one of the almost indispensable components of depression. A noticeable decrease in potency is not accidentally regarded as almost its most important symptom ("symptom of symptoms"), which is detected during targeted research in practically any emotionally unstable patient. It is not by chance that "impotence" as such sometimes turns out to be one of the most frequent erroneous diagnoses. G.S. Vasilchenko also noted that most often a persistent fear of impotence is a symptom of a depressive circle. According to O.P. Vertogradova et al., "A decrease in inclinations (food, sexual, etc.), characteristic of a depressive syndrome, is most pronounced in melancholy and apathetic depressions; )". Research N.Sh. Tatlaeva showed that the clinical picture of sexual disorders is determined by the depth and psychopathological structure of the depressive state. Libido, the level of sexual activity, the quality of erection and orgasm decreased in parallel with the deepening of depressive affect, and this decrease was more pronounced with melancholy and apathetic than anxious variants of depressive disorder. In anxiety-depressive states, in contrast to melancholy and apathetic, short-term episodes of increased sexual desire are observed.
Most modern authors confirm that classic (vital) depression is characterized by pronounced somatovegetative manifestations, including sexual dysfunctions. However, sexual disorders also come to the fore in the case of mild forms of depression (masked, erased, lapped).
It is known that somatovegetative disorders can be the main complaints of the patient with affective pathology. Therefore, with masked somatovegetative disorders, depressions from 1/3 to 2/3 of the patients are observed in doctors of a wide, as well as narrow, non-psychiatric specialists. Some authors point out that latent depression can manifest itself not only by a decrease in sexual functions, but also by hypersexuality, promiscuity and homosexual tendencies of patients. So, D. Renshaw referred to masturbation as manifestations of "latent" depression. V.S. Rothenberg and V.V. Andrianov regarded intermittent night priapism as a sign of latent depression.
Depression is a multilink disorder, the stages of development of which are clinically manifested not only by the deepening of the main symptoms, but also by the modification of the self-awareness and self-esteem of the patients. The most important criterion for the diagnosis of sexual dysfunction (for ICD-10 heading F52) is the subjective feeling of dissatisfaction, depression, anxiety, guilt that occurs in an individual in a situation of sexual contact. In this case, the patient may make complaints that are not really confirmed. In the case when depression is masked by sexological complaints, they are often perceived as purely estimated violations of the type of imaginary sexual. Another typical option is that sexological complaints may dominate, masking affective manifestations. Consequently, the affective disorder itself can manifest sexological dysfunctions. Such depression masked by sexological complaints may not be recognized, and sexual disorders may be regarded as an independent disorder or a symptom of another disease.
It is important that any sexual disorder that has arisen itself has a negative effect on the patient, since the inability to have a full sexual life is one of the most powerful emotional traumas for a man of any age. There are painful personality reactions in the form of depressive affect, aggravating the existing affective disorders and complicating the behavior of therapeutic interventions.
The above is convincing evidence that, in depressive disorders, there is a biological two-way relationship between depression and sexual dysfunction, and problems caused by the psychosexual sphere can be a psychogenic factor in the development and maintenance of an existing depression.
Pathogenesis of sexual dysfunction in depressive disorders
The lack of knowledge of general practitioners about the diagnosis and course of affective disorders leads to prolonged ineffective therapy, as a result of which the depression goes into a chronic course with a noticeable decrease in the level of social and mental functioning and the quality of life of the patient and his family. Another equally significant aspect of this problem is the insufficient attention of psychiatrists to the somatovegetative symptoms of depression, especially at the stage of its reverse development and the development of drug remission, which increases the likelihood of relapse. In the light of the above, it is important to analyze the relationship between somatovegetative (in our case, sexual) and depressive disorders in the pathogenetic aspect.
If we turn to the pathogenesis of depression itself, it is currently being considered from systemic positions, including morphofunctional (neuroanatomical, neurophysiological, neurochemical) and pathopsychological components. Within the framework of the first, much attention is paid to the pathological functioning of the brain structures, in particular the limbic-talamic and hypothalamic-pituitary regions. It has now been established that in depressive disorders, impairments in the production of neuropeptides are detected - hypothalamus releasing factors. Through the pituitary gland, they affect various hormonal functions of the body, causing, in particular, the phenomenon of hypercorticism, which was revealed during depression. If the ratio between glucocorticosteroids and monoamine neurotransmitter system function is normally determined by the nature of the feedback (an excess of cortisol in the blood inhibits the release of corticotropin-releasing factor of the hypothalamus and, accordingly, adrenocorticotropic hormone of the pituitary gland), with depression, their relationships change significantly. At the same time, norepinephrine and serotonin have a direct regulating effect on the secretion of corticotropin-releasing factor. The deficiency of adrenergic neurotransmitters and the associated hypercorticism contribute to the occurrence of depressive disorders by forming a "pathological circle" in the hypothalamic-pituitary-adrenal system with positive feedback. At the same time, the limbic system is the main coordinator, forming an integrative chain through which the cortical centers of emotion regulation send impulses to the hypothalamus, and the hypothalamic impulses are transmitted to the hippocampus. Dysfunction of the reticular formation as an activating system of the brain causes an "energy defect", a decrease in the "biotonus" of the brain mechanisms, which affects the energy component of the libido, causing it to decrease, and, as a result, affects the entire copulatory cycle.
Constitutional or acquired disorders in the hypothalamic-pituitary-adrenal system are reflected in the clinic of depression, as evidenced by the phenomenon of neuroendocrine disinhibition. Depletion of central mediator noradrenergic structures reciprocally causes an increase in peripheral hormonal adrenomedural activity. Thus, a somatic sympathic-tonic syndrome is formed, which causes the inhibitory effect of higher centers on the spinal center of the erectile reflex, blocking the parasympathetic impulses necessary for vasodilation of the penis, as well as an increased sympathetic tone, leads to an increase in the tone of the smooth muscles of the penis, causing difficulty blood flow and, as a consequence, a violation of erection. This affects the neurohumoral component and copulatory cycle. All together causes erectile dysfunction of varying severity, and also leads to disorders of ejaculation (acceleration or deceleration, up to the absence).
In the pathogenesis of depression, a role is played by impaired activity and pineal gland, which lead to the so-called low melatonin syndrome. The deficiency of melatonin produced by the pineal gland disrupts the circadian rhythm of cortisol secretion, explaining the circadian dynamics of the mental state in depressive disorders (mental deterioration in the morning and its improvement in the evening, and this corresponds to the patients' sexological complaints: increased sexual activity in the evening and a decrease or absence morning).
Normal sexual activity is currently defined as an extremely complex psycho-physiological function localized along the hypothalamus-pituitary-sex gonads axis, on the one hand, and having representation in the higher cortical centers, on the other, not to mention the participation of the limbic system. Sexual dysfunctions in mental disorders have a complex pathogenesis, since they are associated not only with the neurodynamic shifts discussed above, but also the previously formed behavioral conditioned reflex stereotypes of sexual behavior relating to all its manifestations - attraction, arousal, orgasm, ejaculation.
The nervous regulation of the sexual function is understood as a dynamic functional system that combines the cellular structures of different levels of the nervous system into a single regulatory mechanism. The combination of brain and humoral components in the functional structure of the libido determines the extraordinary lability of the latter under the influence of not only the general vitality and purely situational factors, but also above all the emotional state of the individual. An erection along with ejaculation are characteristic phenomena of male sexuality, and are regulated mainly by the autonomic nervous system. In affective disorders, regardless of the rhythm of sexual activity, there is always a vegetative imbalance of regulation: either the predominance of sympathicotonia (tachycardia, mydriasis, constipation, etc.), accompanied, as a rule, by acceleration of ejaculation up to ejaculation ante portas; or parasympathicotonia (bradycardia, low blood pressure, sweating, lacrimation, hypersalivation, etc.), accompanied by slow ejaculation until anejaculation.
Systemic sexology explains orgasm as a result of a complex interaction of a number of structural formations located at different levels (pelvic, spinal, diencephalic and cortical). For convenience of analysis, the system concept allows conditional separation from the considered functional unity of two levels - cerebral and segmental. Cerebral - unites all cortical conditioned reflex complexes of the sexual sphere. It includes the cerebral cortex and the regions of the interstitial brain associated with the genital area, including the optic tubercle. The lumbar and sacral parts of the spinal centers of ejaculation with their extraspinal, including earmarked, are referred to the segmental level. In the formation of sexual desire men take part in the same levels as the orgasm, but the degree of participation of each of them is different. If supraspinal (cerebral) mechanisms play the role of instances in orgasm, mainly sensory perception of the final phases of the orgasm and their evaluation, then cerebral formations perform all major tasks during libido formation throughout the entire life cycle.
An important aspect of the violations under consideration is the fact that the superstrong conditioned reflex complexes formed during the pathological process are superimposed on their physiological basis. Natural sexual stimuli turn into a conditioned inhibitor, for example, in an altered physiological state, an attempt made in adverse conditions gives rise to the fear of repeating failure and leads to the fact that each subsequent attempt, with steadily increasing anxiety, is at first less likely, and then completely excludes a favorable completion of intimate intimacy. This in itself at the final stages intensifies the existing affective disorders and forms already new and persistent reactive depressions.
Thus, the pathogenesis of sexual disorders in depression, considered from a systemic point of view, includes both morphofunctional (neuroanatomical, neurophysiological, neurochemical) and pathopsychological components. Mechanisms of suppressing sexuality with reduced affect are due to impaired mental and neuroendocrine components of the copulatory cycle. Also, the basis of the pathological genesis of sexual dysfunctions is based primarily on changes in the neurotransmitter systems, and subsequently on the vegetative, vascular and endocrine levels.
Summarizing the above, we can say that the pathogenesis of affective disorders and sexual dysfunctions is a single and multi-level process. Accumulated evidence suggests that there is a bi-directional relationship between depression and many sexual disorders, and psychosexual-related problems can be a psychogenic factor in the development and maintenance of an existing depressive disorder. This suggests the importance of understanding the pathogenesis of sexual disorders, which is key to their adequate and highly effective therapy. The approach to the treatment of these conditions should be comprehensive, taking into account all components of the disease and aimed not only at the core, but also associated syndromes, without affecting which normalization of impaired functions cannot be achieved. Also, when drawing up a plan of therapeutic effects, it is necessary first of all to analyze the totality of causal factors and to achieve the elimination of all the disease-causing effects that continue their action. Only by providing a pathogenetic approach to therapy can one achieve its effectiveness in sexual disorders caused by depression.
Prevention of erectile dysfunction in patients with metabolic syndrome
Introduction
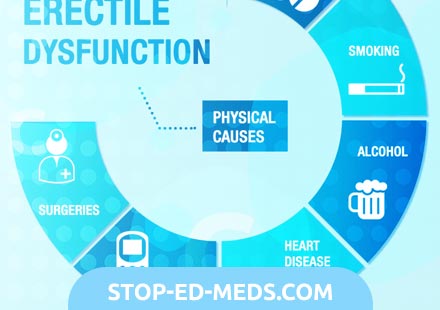
According to modern concepts, metabolic syndrome (MS), which combines the most important vascular risk factors, is one of the most common causes of erectile dysfunction (ED). Moreover, clinical studies have shown an increase in the frequency and severity of ED as the number and duration of MS components increase. Increased severity of ED adversely affects the effectiveness of the therapy, therefore it is extremely important to prevent the development of severe forms of erectile disorders, including in patients with MS.
Erectile dysfunction in men suffering from MS, in most cases are arteriogenic in nature and can be considered as one of the vascular complications of this syndrome. Given that the timely correction of components of MS is considered the main method of preventing its cardiovascular complications, such an approach can help reduce the frequency of ED in these patients. Among the methods of prevention of vascular complications in patients with MS, the main importance is attached to the correction of lifestyle factors and weight loss. The increase in physical activity contributes significantly to the preservation of erectile function in patients with MS, even if it starts in adulthood, which has been objectively proven in a number of epidemiological studies. In particular, it is shown that daily walking for 2 miles for 2 years allows sexual activity to be restored in 33% of obese patients. Correction of other components of MS, including arterial hypertension and dyslipidemia, may require medical therapy. However, by themselves, the drugs used for such therapy can adversely affect erectile function, which requires a selective approach in the choice of drugs.

The emergence of new highly effective oral medications for the treatment of ED makes it possible to use them as a prophylactic agent in patients with risk factors. One of them is the domestic drug Impaza, the mechanism of action of which is associated with increased activity of the enzyme endothelial NO synthase, which plays an important role in the development of erection.
To date, in the available literature, we have not found data on the use of this drug for the treatment of ED as prevention of erectile dysfunction in patients with MS. In addition, the volume and nature of preventive measures aimed at preventing the development of ED in men with MS have not yet been determined.
The above data, in combination with the potential reversibility of the pathological changes underlying the pathogenesis of ED in patients with MS, underscore the possibility of preventing erectile dysfunction, which led us to conduct our own research.
Materials and methods
The study included 152 patients with MS (mean age 47.8 ± 12.18 years), at the time of the survey had normal erectile function. All patients underwent a comprehensive clinical examination, which included routine research methods (history taking, examination, clinical and biochemical blood tests) and special methods for the diagnosis of ED and MS. To evaluate erectile function, we used the questionnaire of the international index of erectile function (ICEF). For the diagnosis of MS, the criteria of the National Cholesterol Educational Program were used. The presence of a patient with at least 3 of 5 proposed criteria was regarded as MS: abdominal obesity, hypertriglyceridemia (> 1.7 mmol / l), reduction of high-density lipoprotein (HDL) (<1 mmol / l), arterial hypertension (> 130/85 mmHg.), increasing the concentration of fasting blood glucose (> 6.1 mmol / l).
To evaluate endothelial function, post-compression tests on the brachial and cavernous arteries were used and the level of asymmetric dimethylarginine (ADMA) was determined using enzyme immunoassay (CardioS Vasics Medical Science Labs). The concentration of ADMA above 0.573 ?mol was regarded as a high risk, from 0.062 to 0.572 ?mol as moderate risk, and below 0.062 ?mol as its absence. The level of free testosterone in the blood plasma was investigated by enzyme immunoassay.
Analysis of clinical data was performed using standard statistical methods using Microsoft Excel personal computer software and Statistica 6.0 software.
Since all patients included in the study had several vascular risk factors, they could develop ED in the future. Therefore, after the initial examination, patients were monitored dynamically, and the preventive potential of various treatment methods used to correct metabolic disorders and ED was evaluated.
Patients, depending on the received therapy, were randomized into 3 groups: 1st - without correction of MS therapy, obtained before the start of the study; 2nd - only MS therapy was corrected; 3rd - Correction of MS therapy was carried out and Impaza was prescribed for the prevention of ED. The follow-up period was 12 months, but the monitoring of indicators of MS (anthropometry, examination, biochemical blood tests) and evaluation of erectile function were performed every 6 months. Comparing the frequency of occurrence of ED in different groups, we were able to assess the role of different types of MS treatment in the prevention of erectile disorders.
In the 1st and 3rd groups, there were 51 patients each, and in the 2nd - 50 patients. By the time the study began, 74.5% of patients in the 1st group regularly received hypotensive, 19.6% - hypoglycemic, 3.8% - lipid-lowering therapy. Of the antihypertensive drugs, non-selective -blockers (33.3% of patients) and angiotensin-converting enzyme inhibitors (ACF) (15.7% of patients) were used most often. 11.8% of patients with arterial hypertension did not receive systematically antihypertensive therapy. To reduce blood sugar levels, 19.6% of patients took glucose-lowering oral medications from the group of sulfonylurea derivatives and biguanides. Despite the fact that 80.4% of patients in the 1st group had dyslipidemia, only 3.9% of them received lipid-lowering therapy in the form of an inhibitor of cholesterol synthesis (simvastin).
Patients of the 2nd group were treated for all metabolic disorders. For weight loss, dietary recommendations and metered exercise were mainly used. After consultation with a cardiologist in this group, non-selective -blockers (atenolol - 9 patients) and thiazide diuretics (hypothiazide - 6 patients) were taken, taking into account their negative effect on erectile function, with drugs from the group of ACE inhibitors (enalapril - 4 patients), calcium antagonists channels (amlodipine - 5 patients) and selective -blockers (bisoprolol - 6 patients). Correction of the blood glucose level in 8 patients with type 2 diabetes mellitus (DM) was performed using glucose-lowering drugs, and in 2 patients insulin therapy was used. 38 men with insulin resistance were prescribed metformin at a dose of 500 mg per day to increase the sensitivity of tissues to insulin. Lipid level correction in 45 patients was carried out with a diet (according to the recommendations of the European Cholesterol Program), which was combined in 8 of them with taking statins. In 3 patients, low levels of free and total testosterone were combined with a decrease in libido, and they received the testosterone drug Sustanon-250 in the form of intramuscular injections 1 time in 3 weeks. Patients of the 3rd group for the correction of lifestyle factors and metabolic disorders used the same treatment principles used in patients of the 2nd group. A significant difference in the number and nature of the therapy obtained in the correction of metabolic disorders between the 2nd and 3rd groups was not found. For the purpose of drug prevention of ED in patients of the 3rd group, the domestic preparation Impaza was additionally used. Patients received impazu daily in the form of tablets under the tongue, regardless of the meal for 12 months.
Results
A comparative analysis showed that the groups formed are comparable in age and baseline anthropometric indices and do not have significant differences. Control tests after 12 months showed that patients of the 2nd and 3rd groups achieved positive results in weight loss. Significant differences in weight loss between the 2nd and 3rd groups were not found. In patients of the 1st group, where they did not use special methods for the correction of overweight, there was no significant reduction in BMI and decrease in waist circumference during the observation period.
The levels of systolic and diastolic blood pressure (BP), which were initially comparable in all groups, significantly decreased after treatment in the 2nd and 3rd groups. Irrational selection and unsystematic reception of antihypertensive drugs did not allow patients of the 1st group to achieve the normalization of systemic blood pressure, and in some patients it was noted an increase.
The number of patients with type 2 diabetes in the 1st group for 12 months increased almost 2 times, and in the 2nd and 3rd groups remained unchanged. The treatment aimed at increasing the sensitivity of tissues to insulin, the number of patients with insulin resistance and hyperinsulinemia in the 2nd and 3rd groups, but to the greatest extent in the 3rd group significantly decreased, and in the 1st group, on the contrary, increased .
Diet therapy and statin administration improved the indicators of fat metabolism in the 2nd and 3rd groups. Under dynamic observation in these groups, indicators of total cholesterol, triglycerides and atherogenic coefficient decreased to the same extent, and the level of HDL cholesterol increased, approaching normal values. In patients of the 1st group, the dynamics was inverse, that is, an increase in the level of atherogenic lipids and a decrease in HDL concentration was observed.
Despite the fact that the initial average values of the index of postcompression increase in the diameter of the cavernous arteries (AUC) in all groups corresponded to normal values and did not have significant differences, after follow-up after treatment these indicators in patients of the 2nd and to a greater degree of the 1st group significantly decreased . The average values of the HACK in the 3rd group did not change during the observation period. The degree of post-compression increase in the diameter of the brachial artery in patients of the 1st group also significantly decreased, and in patients of the 2nd and 3rd groups increased.
In the 2nd and 3rd groups, the number of patients in whom the level of ADMA corresponded to a high risk decreased by almost 3 times, and in group 1 did not significantly change.
Correction of metabolic disorders in patients of the 2nd and 3rd groups was accompanied by an increase in the level of total and free testosterone. However, the degree of increase in the concentration of androgens between these groups revealed no statistically significant differences. In patients of the 1st group, the level of sex hormones decreased).
The average indicators of the erectile function on the ICEF scale initially in all groups were above 26 points, which corresponded to normal values. After 12 months, patients of the 1st and 2nd groups showed a significant decrease in the number of erectile function scores on the ICEF, whereas in the 3rd group, these figures did not change. Patients of the 1st group had more pronounced changes in the indicators of erectile function and were less satisfied with the quality of sexual acts.
The most common ED occurred in patients of the 1st group. More than half of these patients (52.94%) noted a deterioration in the quality of both spontaneous and adequate erections. In patients with the 2nd and 3rd groups, ED developed much less frequently (in 16 and 5.88% of cases, respectively). The number of patients with moderate ED prevailed in the 1st group. All patients with ED were in the age group older than 50 years.
Discussion
Prevention is a key method of dealing with MS. The first studies show that eliminating risk factors in people prone to developing MS can reduce the frequency and severity of ED, as well as other vascular complications, including type 2 diabetes. In addition, in recent years, works have appeared that eliminating risk factors for cardiovascular diseases by non-medicinal methods leads to a decrease in the likelihood of developing ED or reducing its severity.
Dynamic observation over 12 months showed that the degree of compensation for existing metabolic and vascular disorders depends on the nature of the treatment. Since not all patients of the 1st group received adequate and complex therapy during the observation period, the main components of MS progressed and led to a significant increase in the number of patients with type 2 diabetes, insulin resistance and compensatory hyperinsulinemia. The lack of rational therapy contributed to the emergence of more severe disorders of the lipid profile, especially an increase in the concentration of triglycerides, which in turn increased the severity of the existing vascular disorders. During the observation period, in group 1, the number of patients with clinical and biochemical signs of endothelial dysfunction increased dramatically, which, apparently, led to the occurrence of erectile dysfunction in more than half of the patients. The level of total and free testosterone in them also decreased, which increased the severity of ED.
The high effectiveness of pathogenetic therapy in the 2nd and 3rd groups indicates the need for correction of all metabolic disorders in patients with MS. In these groups, with adequate treatment, the BMI decreased almost equally, the waist circumference, the levels of systolic and diastolic blood pressure, and the lipid profile improved. In these patients, ACE inhibitors were more often used as antihypertensive drugs, which increase the sensitivity of tissues to insulin. Acceptance of ACE inhibitors along with normalization of lipid metabolism and the use of metformin helped reduce the severity of insulin resistance and prevented a further increase in the number of patients with type 2 diabetes in the 2nd and 3rd groups. Reducing the severity of visceral obesity could contribute to increased levels of sex hormones in the 2nd and 3rd groups.
Clinical evaluation of postcompression changes in the diameter of the brachial and cavernous arteries before and after treatment allowed us to study the effect of different types of therapy on endothelial function in patients with MS. Correction of metabolic disorders in the 2nd and 3rd groups was accompanied by an improvement in the endothelial function on the brachial artery and a decrease in the level of ADMA. However, in the 2nd group, in contrast to the 3rd, the number of patients with endothelial dysfunction of the cavernous arteries increased significantly, which led to the development of ED in 8 (16%) cases. The results of the evaluation of indicators of an AUDA demonstrate the improvement of endothelial function in the penis in patients of the 3rd group. This is also indicated by the decrease in the number of men with endothelial dysfunction of the cavernous arteries in this group. This fact may indicate a beneficial effect of impazy on the endothelial function of the cavernous arteries. Along with complex therapy, long-term prophylactic administration of this drug significantly reduced the risk of ED in patients with MS (5.88%). The reason for choosing this particular drug was a number of factors, one of which is effectiveness, which has been repeatedly proven in clinical trials, including placebo-controlled ones. The effectiveness of impasi is mainly observed in patients with a mild degree of ED, with arteriogenic disorders, the most common in MS. In addition, the mechanism of action of impasi is associated with the stimulation of the activity of the enzyme endothelial NO synthase, which is actively involved in the regulation of endothelial function, which was also important for our patients. Other advantages of this drug are its relatively low cost, absolute safety and good tolerability, which is important for patients with MS.
However, despite the use of complex therapy and the use of special drugs for the treatment of erectile dysfunction, not all patients with MS managed to prevent the occurrence of ED. This fact once again demonstrates the heterogeneity of patients with MS and dictates the need for a differentiated approach to their treatment and prevention of MS.
Conclusion

For the prevention of ED in patients with MS, it is first necessary to eliminate the existing adverse lifestyle factors and correct all metabolic disorders. These activities can reduce the severity and stabilize the course of MS, reduce the likelihood of an erection disorder in this category of patients. However, to reduce the likelihood of developing erectile dysfunction in this category of patients, in addition to correcting metabolic disorders, it is necessary to take special medications used to treat ED.
